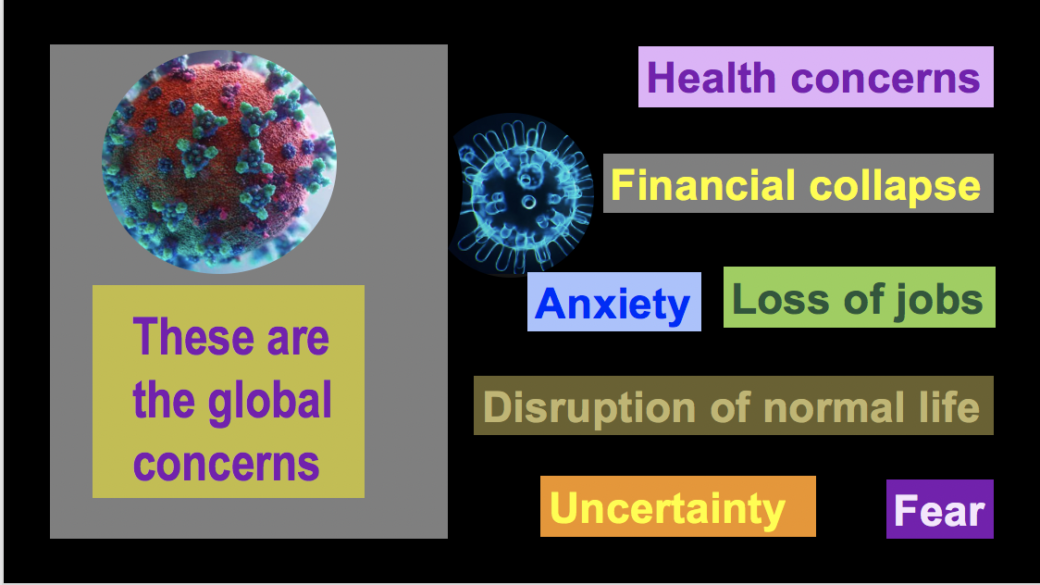
It is now less than three months since I treated my first patient with Covid-19 in March 2020. Life has become very different since then. We are passing an uncharted territory in our planet’s history, as the Covid-19 crisis has dragged the global economy into a spectacular collapse. It brought the healthcare systems across the nations to the brink. The surge in patient numbers in the hospitals, prolonged hospital stay, front-line worker’s concerns for their safety from the virus all pushed the healthcare workers to the edge of exhaustion and burnout.
Three months into the pandemic, my daily struggle to fight Covid-19 became a personal one. All my strategies to evade the virus finally failed. I got infected with the dreaded foe, the Coronavirus.
Today is July 27, 2020. I am writing this as the number of US death from Covid-19 approaches 150,000, and the death count surpasses 650,000 globally. In the US, in the northeastern states of New York, Pennsylvania, and New Jersey, cases of Covid-19 have somewhat calmed down. The epicenters have now shifted to the southern states and the west coast. California, Florida, Texas, and Arizona are the current top hot spots for the infection where the pandemic continues to unfold its vengeance, causing suffering and death.
My rituals of repeated wiping and cleaning start first thing in the morning. Inside the hospital, we are obsessed with the virus in everything we touch and the air we breathe. Such excessive worries coupled with repeated wiping and cleaning habits would be considered obsessive-compulsive disorder (OCD) on regular days. These are not normal, ordinary days. In the Coronavirus era, these are life-saving practices no physician can afford to get around. After numerous N-95 masks, dress-ups with protective gears in carefully orchestrated layers, and then peeling them off one by one, the virus finally penetrated my defense!

Loss of smell, fever and headache
I came home from the hospital that day with severe body aches, a nasty headache, and chills. I checked if I could smell, which was a daily practice I have been doing since the pandemic began. Loss of smell sensation could be an early symptom of Covid-19. I tried to smell a perfume from my wife’s collection. I could not smell it, as if I was trying to smell water! I checked my temperature; it was 101F. The symptoms were too familiar! Without having a second thought, I said to myself: O God, I have it!! I decided immediate isolation from the rest of my family.
The brush of Coronavirus
The following morning, I woke up with a 102 F fever, having chills, headaches, and severe exhaustion. I called my hospital and canceled my scheduled hospital assignments. I drove to the hospital outpatient turned Covid-19 testing center. People were waiting inside their cars for the test. A nurse in full PPE gear came up to me, did a quick heart and lung exam while I was inside my car. The actual test involved a swab that went deep inside my oral cavity. The department of county health called me the following day. I had covid-19.
A peek inside the isolation
Suddenly as if I became radioactive! I knew that no one should come near me or touch me, or even breathe around me. I am now in complete isolation in quarantine. The venue for my isolation was my bedroom with an attached bathroom. I kept my door closed all the time. My wife used to leave my food and drinks on a small table placed outside my door. After making sure that she has left, I stepped outside the room while wearing my N-95 mask, brought the food inside, and closed the door behind me. I used to do FaceTime and zoom chat with my wife, children, and friends, my only connection with the world outside my room for the weeks to come.
The magic of the yellow turmeric drink
My wife found a herbal remedy for me after searching Dr. Google. It was the yellow-colored turmeric drink with its exotic wild smell, which she added to my daily menu. Turmeric is a herb used as a yellow food coloring agent in Indian-Bangladeshi food. It helps inflammation in Covid-19 patients, as my wife found out in her Google search. The fluorescence of the bright yellow magical turmeric drink, its wild smell, and unfriendly taste will always be with me as part of my Covid-19 memories!

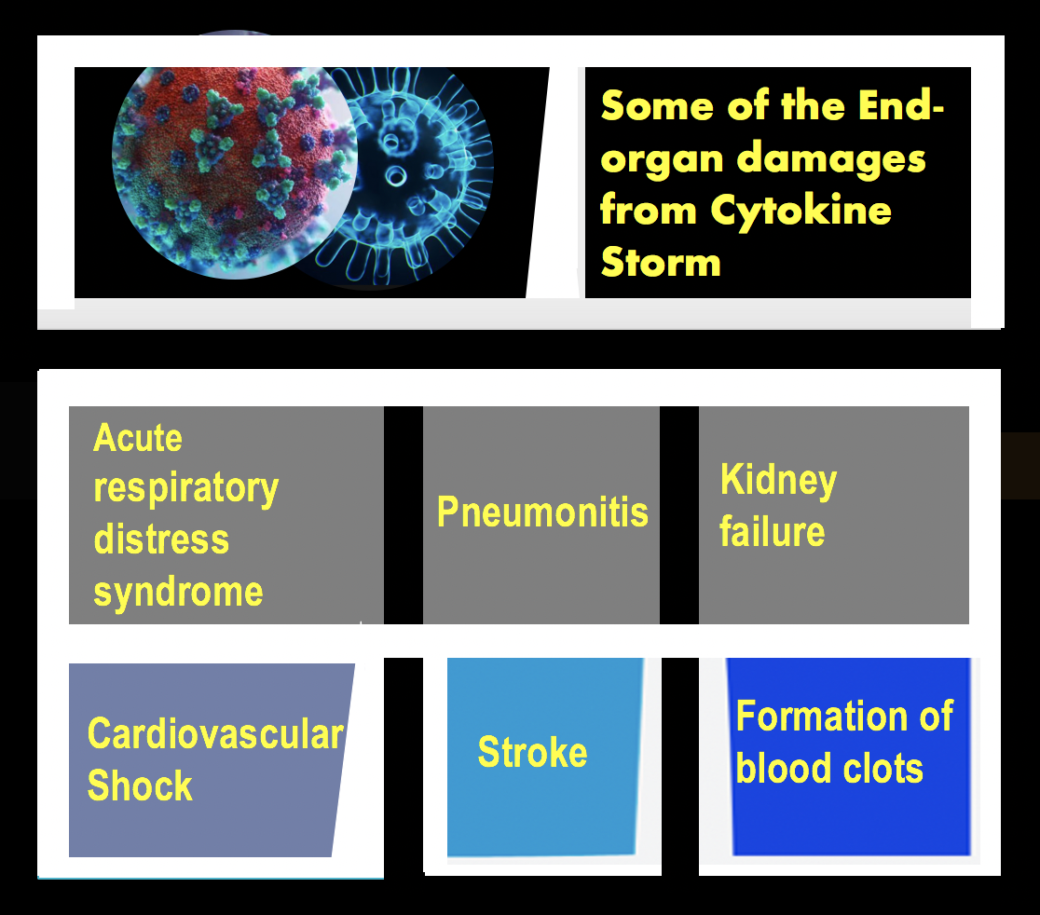
Over the next several days, I continued having waxing and waning fever. My oxygen levels stayed within the normal range—my smell sensation returned to normal by the fourth day. My biggest concern was whether I would face a Covid-19 cytokine storm resulting from a devastating burst of self-destructive antibody production by the body’s defense mechanism. Cytokine storms may occur around 7-10 days from the beginning of the infection.
There came the storm
On day seven, my symptoms changed towards worse. I started getting violent coughing spells, so severe that I could hardly talk. I spent the night sitting on my bedside sofa, with my eyes full of sleep but unable to rest due to endless assaults from severe coughing spells. Early in the morning, my oxygen level dropped to 92% from 98% the day before. I knew this was my time to head towards the hospital. The nearest hospital was within fifteen minutes’ driving distance from my home. Driving a personal vehicle will take less time than getting an ambulance for transport.
What is a Cytokine Storm?
Our over-active immune response can induce a Cytokine storm. A regulated immune response organizes chemical reactions to clear the infection from our body by releasing chemicals, including interleukins, interferons, tumor necrosis factors, and other mediators. These mediators are bio-chemical agents essential to destroy infectious agents from our systems. The overproduction of the same chemical mediators can target our cells and ruin our body tissues. Cytokine storm is not unique to COVID-19. Cancer patients receiving immunotherapy and patients with autoimmune diseases can experience similar symptoms.
My trip to the hospital
In the early hours of the morning, I started feeling a gradually evolving mental fog. My oxygen level, which was trending lower, and my lack of sleep pushed me to daze, with my mind getting hazy. I watched Tamim, my older son, wearing an N95 mask and get into the driving seat. I was concerned about Tamim’s exposure to Covid-19 from me. He insisted that he would drive me to the hospital. I saw my wife and my eleventh-grader son Zayd standing outside the house. They were waving bye to me as I left the house in the shadowy darkness of the early morning. Their faces were half-covered with masks, concealing their anxiety, emotions, and concerns.
I did not anticipate any surprise in a Covid-19 respiratory isolation room. I have been in similar rooms too often, seen too many people gasping for breath. The concerns about the disease’s potentially deadly nature didn’t affect me when I was getting admitted to the hospital. There was no feeling of impending doom within me. I just wanted to feel better and my cough to go away.
The misery of isolation
Every Covid-19 patient has a unique story to tell. They suffer behind the scenes, isolated from the rest of the world. They go through physical sufferings and psychological devastation in a lonely cubicle. They struggle to breathe and try to stay alive. The only people they come by are the health care providers with protective gear; the only voices they can hear are the muffled voices from behind the N-95 masks. They feel scared, and they want their family to be by their side, comforting them, holding their hands. Indeed, they do not get those desires fulfilled, even though some of them approach their last breath.
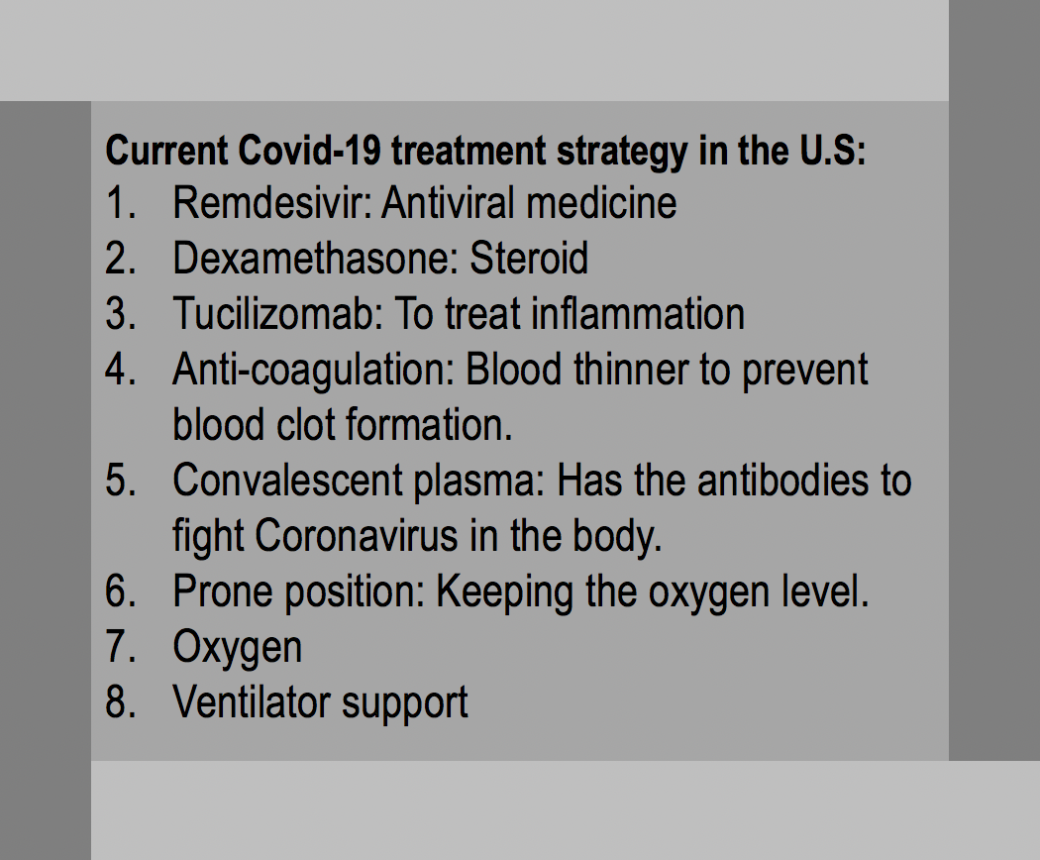
The treatment strategy
At the beginning of the pandemic, Covid-19 was a little-known clinical entity for the practicing physicians. As the weeks and months have passed, the results of new studies were available. These helped to develop a more evidence-based structured treatment strategy, which is still evolving. Not surprisingly, there have been frequent and frantic changes in the protocols to treat Covid-19 since the beginning of the pandemic.
Remdesivir: An old medicine, a new hope
I started receiving a five days course of Remdesivir, an antiviral drug. It was the first week of Remdesivir being available in the U.S for treatment of Covid-19. My fantastic colleagues and my daughter, a Pulmonary Critical care fellow, were valuable advocates for my management when the healthcare institutions were overwhelmed with Covid-19. Desperate attempts by my co-working physician, who I am forever thankful to, helped me in the difficult time by ensuring that the medicine, which was in extremely short supply at the time, was available for me.
Treating Covid-19: evolving strategies, July 2020
Keeping up your oxygen
My lowest oxygen level was around 91%. I was not in an acute respiratory failure, though I felt It was rapidly approaching. I could hardly sleep because of vivid nightmares, which accompanied my fever with drenching cold sweats and cough. Getting used to sleeping in a prone position was not easy for me at the beginning. I had to be familiar with the prone position to keep my oxygen level normal and help my symptoms.
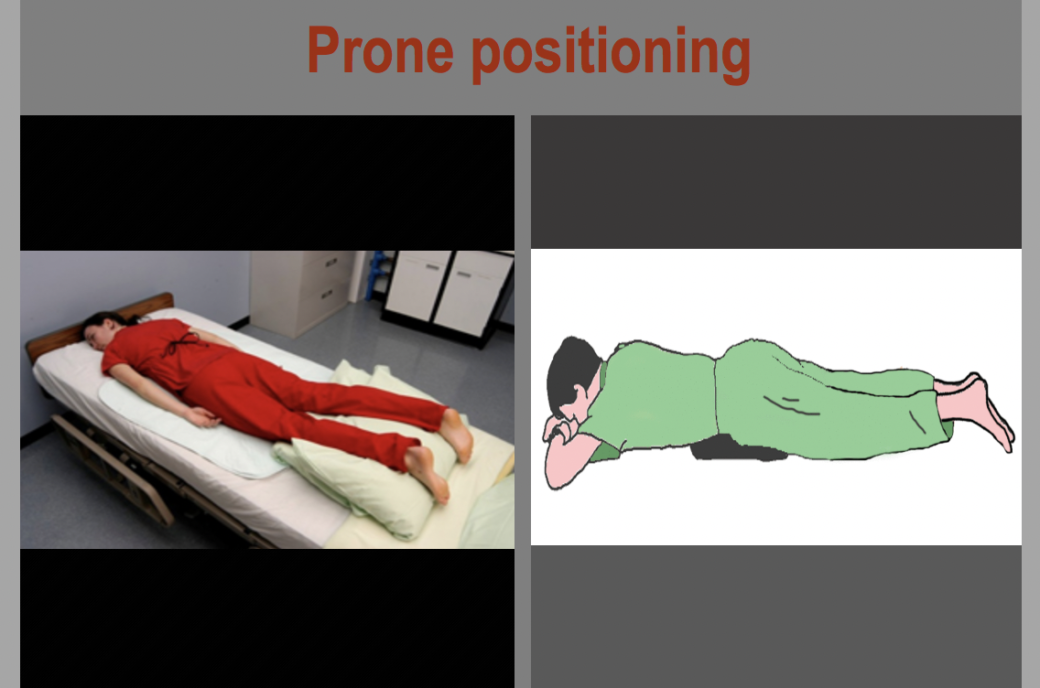
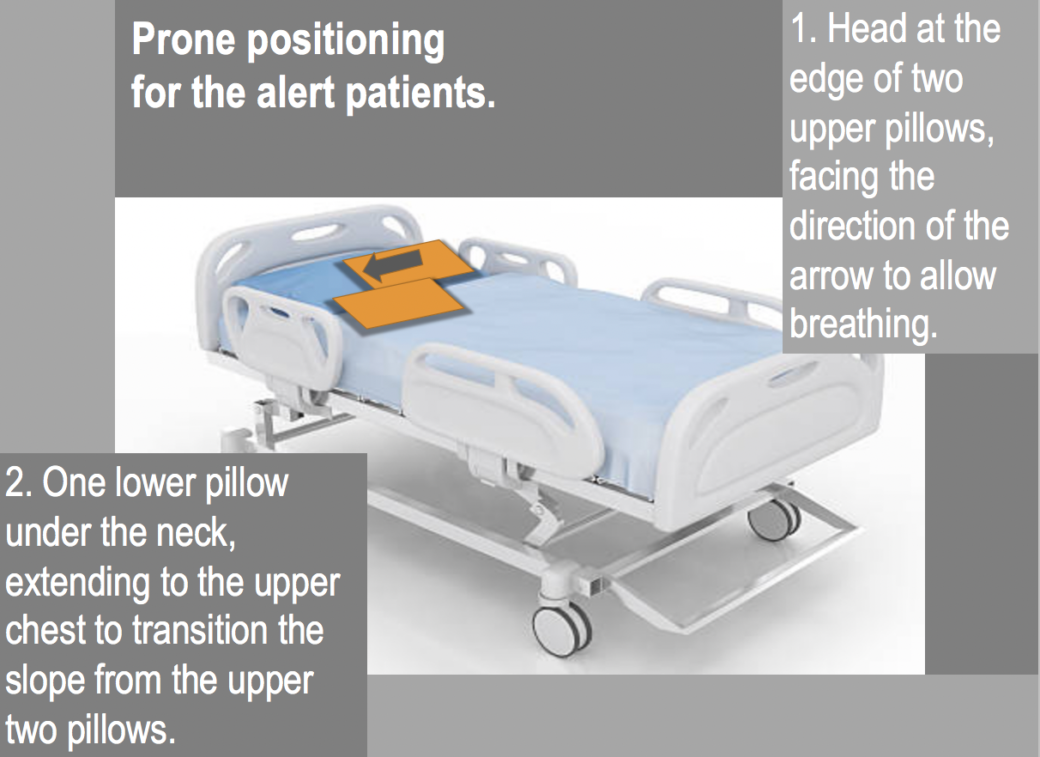
Prone position to stay alive
The prone positioning is lying on the chest and the belly, with the head turned to the side. The positioning is vital to help the oxygen level in a covid-19 patient. The goal is to optimize lung tissue function. Prone positioning decreases the lungs’ pressure from the heart’s weight and supporting structures and the weight of the swollen edematous lungs themselves.
Customized pillows are now available to place patients in a prone position. I used two standard pillows under the head and one pillow underneath my neck, extending to the upper chest, my belly being on the bed. I had to adjust the relative position of the pillows to get comfortable. Deep breathing exercises with incentive spirometry and lying in a prone position are two vital actions that can help oxygen level and avoid the need for ventilator support.
Living means being thankful
I was in the hospital for seven days. Those days in the hospital gave me a new appreciation for the simple life-gifts I always took for granted. I learned to cherish each normal breath as an astounding grace to me, making my life possible. The comforting words and good wishes from my family, friends, and colleagues reminded me of how precious those words and loving expressions are in our life. While suffering from a life-threatening disease that does not have effective treatment at the time, the love and compassion from the family and friends seem to be the pieces of straw someone wishes to hold onto and remain afloat.

Life goes on
I left the hospital on the 7th day. I continued feeling extreme exhaustion with a continued cough. I pushed myself with varieties of aerobic activities, including my favorite one, jogging. I felt blessed. My shortness of breath with minimal exertion improved promptly and returned to an average level in a few weeks. I was physically able to return to work two weeks after coming out of the hospital.
I couldn’t feel more proud and privileged to be part of my front-line combat team. My colleague doctors and nurses, who were rejoicing my comeback, expressed their relief, some with smiles and some with a touch of tears. It was as if a war buddy getting out of lethal combat alive in one piece. There were no shaking hands or hugging, of course. We have not forgotten that it is the Covid-19 era; there is not much room for human emotions.
My wiping and cleaning rituals resumed as intense as it was at the beginning of the pandemic. Entrances and exits to patient’s rooms remained as complicated as they were. We knew that any wrong moves from us while peeling off and handling our PPE gears could cause infection to others, and we can cause someone or ourselves to end up in a ventilator. It is the reality now and will continue to be the reality for the foreseeable future.
The survival
It is July 15th, 2020, today. I am reflecting on my brush with Covid-19 while the world is in a mode to survive and struggle to remain afloat. The nations are trying to tackle the multifaceted challenge that Covid-19 has created. Researchers and the pharmaceutical industries are pursuing the vital task of finding a vaccine for the virus at an unrelenting speed. Unfortunate politicization of the pandemic in the U.S. and some other countries have destroyed the global alliance needed to fight this pandemic crisis.
Like all other Covid-19 survivors globally, I hope that people realize this disease’s destructive potential and take appropriate preventive measures. Like all other passionate healthcare providers, who are taking the risk of their own lives to save others from dying, I hope that people follow the lead of medical science to tackle this deadly disease, not their political faith. It is the appropriate approach from someone who is a conscious citizen and a good human being.
Be the first to comment